Academic Courses
FACULTY OF NURSING
Click here to access Unit one Content..
Topic 1.0: CVS Pathology
- Learning Outcomes
- At the end of the unit the learner should be able to: -
- 1. Describe congenital cardiac anomalies and their effects on cardiac function
- 2. Explain the aetiology, pathophysiology and features of cardiovascular disorders
- 3. Explain and interpret the investigations in cardiovascular diseases/disorders
- 4. Describe complications of cardiovascular disorders/disorders
- Unit Outline
- Introduction – Review of Anatomy and Physiology
- The Heart (Congenital Heart Diseases, Cardiac Failure, Manifestations of Cardiac Failure, The Pericardium [Pericarditis], Myocardium [Cardiomyopathy, and Myocarditis], Ischaemic Heart Disease [Angina pectoris and Myocardial infarction], Valvular Heart Disease, Acute Rheumatic Fever, Rheumatic Heart Disease and Infective Endocarditis)
- a. Arterial Blood Vessels - hypertension, hypertensive Heart Disease (systemic and pulmonary), atheroma and Artherosclerosis, aneurysms
- Venous Blood Vessels - varicosities and haemorrhoids and tumours of blood vessels
Click here to access Unit one Content..
Topic 1.1: Review of Physiology & Anatomy of Cardiovascular System
Learning Outcomes
The student should be able to: -
1. Describe the structure of the organs of the cardiovascular system
2. Describe functioning of the cardiovascular system
3. Describe the structure and function of the heart
4. Describe factors that are important in normal heart function
1.0. INTRODUCTION
2.0. THE HEART
2.1. Introduction
The function of the heart is to pump sufficient oxygenated blood containing nutrients, metabolites and hormones to meet the moment to moment metabolic needs and preserve a constant internal milieu. The heart has three muscles layers - endocardium (inner muscles of the heart, myocardium (provides contractile force to push blood) and pericardium (outer covering). The heart has 4 valves namely the aortic, pulmonary, tricuspid and the mitral valves. Heart muscle has two essential characteristics of contractility and rythymicity.
The conducting system contains specialized cells for initiation and transmission of signals in a co-coordinated manner. It comprises the Sino-atrial node (SAN), the atrio-ventricular node (AVN), the Purkinje tissues (fibres) and the bundle of His.
Physiological function of the heart is maintained by healthy muscles, efficient valves, the conducting system and co-ordination of chambers and normal peripheral resistance
.Diagram 1.1: Normal Heart

The heart has three major types of cardiac muscle namely the atrial, ventricular and the specialized excitatory and conductive muscles.
The Cardiac muscle as a syncytium
The heart muscle has many cells connected in series with intercalated discs with specialized structures such as fascia adherens (mechanical links), mascula adherens /desmosome (lattice structure and site for cytoplasmic filaments) and gap junction (makes the adjacent cells loose and is permeable to ions). The heart has two separate syncytiums namely the atrial and ventricular syncytiums separated by a fibrous tissue.
All or Nothing Principle
Synctial arrangement and interconnection of the myocardial muscle cells allows stimulation of any single atrial fibre to cause action potential to travel over the entire atrial muscle mass. The same holds for the ventricles. If the A-V bundle is intact the action potential spreads from the atria to the ventricles. This is the All or Nothing Principle.
2.3. The Cardiac Cycle
Phase I – Atrial Contraction
This is the period of rapid refilling of ventricles in the first 1/3 of diastole. There is diastasis, which is the slow movement of blood into the ventricles in the middle of 1/3 of diastole and atrial contraction pushes more blood into the ventricles (20 – 30% of ventricular refilling) in the last 1/3 of diastole.
Phase II – Isovolumic Ventricular (Isometric) Contraction
Period of emptying ventricles during the beginning of ventricular contraction when no emptying takes place hence the name isovolumic or isometric (i.e. is there is no increase in tension of muscle but no shortening of muscle fibres)
Phase III – Ventricular Systole – Period of ejection
Period of ventricular systole when there is fast and slow ejection of blood. Left ventricular pressure rises slightly above 80 mmHg and right ventricular pressure rises slightly above 8 mmHg forcing open the mitral and tricuspid valves respectively; this is fast ejection that accounts for 70% of ventricular emptying. There is the period of slow ejection that lasts the last 2/3 of systole.
Phase IV – Period of Isovolumic Ventricular (Isometric) relaxation
Ventricular relaxation begins allowing ventricular pressure to fall. Increased pressure in the distended arteries pushes blood back towards the ventricles closing the aortic and pulmonary valves. The ventricular muscles contract but the ventricular volume stays – isometric relaxation.
Phase V – Ventricular Diastole Relaxation
The period of ventricular diastole relaxation overlaps with atrial contraction.
3.0. CARDIAC OUTPUT
The normal cardiac output for young healthy male adult is 4 – 8 litres/minute (average 5.6 litres/min) with females at 10% less. Five basic mechanisms controlling cardiac output include heart rate, ventricular filling pressure, ventricular distensibility, systemic vascular resistance and ventricular contractility. Cardiac output (CO) = Heart rate (HR) x Stroke volume (SV) of the left ventricle
The Stroke volume
Stroke volume is the diastolic volume of the ventricle minus the volume of blood in the ventricle at the end of systole. Stroke volume output is the amount of blood emptied by the ventricles during systole (usually 70 mls). The Cardiac Index (CI) is the cardiac output per square metre of body surface area. The normal is 3.0 litres/minute and changes with age.
Ejection Fraction
End-diastolic volume is the volume of blood in the ventricles at the end of diastole when the filling of ventricles increases volume of each ventricle to 120 – 130 mls while the End-systole volume is the blood remaining in the ventricles at the end of systole (usually 50 – 70 mls).
Ejection Fraction = 70 x 100 = 58.3% (60%)
120
4.0. THE LAWS
1. Poiseulle’s Law Blood flow = Pressure x diameter of blood vessel
Length of vessel x viscosity of blood
2. Starling’s Law – increase in dilatation leads to increased filling, contraction and stroke volume
3. Frank-Starling – within physiological limits, the heart pumps all the blood that comes to it without allowing excessive damming of blood in the veins. The greater the heart is filled during diastole, the greater will be the amount of blood pumped into the aorta.
4. Laplaces Law – the circumferential force tending to stretch the muscle fibres in the vessel wall is proportional to the diameter of the muscle x the pressure inside the vessel (F = D x P). The wall tension require to counteract a given pressure in a spherical cavity is proportional to the radius of the cavity.
Click here to access Unit one Content..
Topic 1: Summary
PRINCIPAL MECHANISMS OF CARDIOVASCULAR DISEASE
Many diseases can involve the heart and blood vessels but generally cardiovascular dysfunction results from five main mechanisms: -
- Failure of the pump
- An obstruction to flow
- Regurgitation flow
- Disorders of cardiac conduction
- Disruption of the continuity of the circulatory system
Click here to access Unit one Content..
Topic 2.1: Congenital Heart Diseases
Learning Outcomes
At the end of the lesson the learner should be able to: -
- Explain the pathogenesis of congenital heart diseases
- Classify congenital heart diseases
- Outline the manifestations of congenital heart diseases
- Describe the effects of congenital heart diseases
Click here to access Unit one Content..
Topic 2.2: Introduction to Congenital Heart Diseases
INTRODUCTION
Congenital heart disease is the abnormality of the heart or blood vessels present from birth. It is the most important cause of heart disease in the early years of life and the incidence is higher in premature infants. Cardiac malformations occur during the stage of cardiac development (3rd - 8th week of gestation). Cardiac abnormalities could be incompatible with intrauterine life, manifest shortly after birth when foetal circulation changes to the postnatal circulation, cause cardiac malfunction only in adult life or be entirely innocent.
Congenital anomalies are morphologic defects that are present at birth. These anomalies may occur are malformations, disruptions, sequences and syndromes.
Malformations are primary errors of morphogenesis where there is an intrinsic abnormal development process. They are as a result of multiple causes.
Disruptions result from secondary destruction of an organ or body region that was previously in normal development. Results from extrinsic disturbance in morphogenesis.
Deformations result from extrinsic disturbance of morphogenesis through local or generalized compression of the growing foetus by abnormal biomechanical forces e.g. uterine constraints such as maternal factors (which ones?) and foetal factors (such as?).
Sequence – a pattern of cascade anomalies (examples?)
Syndrome - collection of congenital anomalies
DEVELOPMENT OF THE HEART
The remarkable development of the heart occurs in 6 – 7 days but becomes obvious at day 18 or 19 in the cardiogenic area of the mesoderm layer where a paired mass of specialized cells called the heart cords form. After a short time a hollow centre develops in each cord to form a heart tubes. The heart tubes begin to migrate towards each other during day 21 and soon fuse to form a single median endocardial heart tube. The process of fusion is accompanied by dilatations and constrictions of the tube so that when fusion is completed during the 4th week five distinct regions can be seen. These regions are the truncus arteriosus, bulbous cordis, ventricle, atrium and sinus venosus.
- Idiopathic/unknown (90%)
- Genetic – arise from karyotypic aberrations, gene mutations and multifactorial inheritance. Examples - chromosomal abnormalities e.g. Trisomy 21 (Down’s syndrome)
- Environmental factors such as infections in the mother during pregnancy e.g. rubella, drugs and alcohol and cigarette smoking, radiation, maternal diabetes
- Multifactorial causes
Click here to access Unit one Content..
Topic 2.3: Pathology of congenital Heart Diseases
- PATHOGENESIS
- The timing of prenatal teratogenic determines the occurrence and type of anomaly produced. The embryogenic period which takes first 9 weeks (early - 1st 3 weeks) and foetal period (10 weeks to birth) determine the outcomes as organogenesis occurs mainly during embryogenic whereas during the foetal period there is growth and development of organs with reduced susceptibility to teratogenic agents but susceptible to growth retardation.
- CLINICAL EFFECTS/FEATURES
- Children with significant congenital anomalies have disturbance in the haemodynamics of blood flow, failure to thrive, cyanosis, increased risk to recurrent or chronic infections and high risk of infective endocarditis.
- CLASSIFICATION
- Malposition of the heart
- Shunts (Cyanotic Congenital Heart Disease) - Left-to-right shunts and Right-to-left shunts
- Obstructions (Obstructive Congenital Heart Disease)
- MALPOSITIONS
- Ectopia Cordis
- This a birth defect in which the abnormally located outside the thoracic cavity and has defective heart muscles and coverings. Most commonly the heart protrudes outside the chest through a split sternum and less often the heart may be situated in the abdominal cavity or neck. The condition is fatal in first days of life. It is associated with other malformations such as Tetralogy of Fallot, pulmonary atresia, atrial and ventricular septal defects, and double outlet right ventricle. Other non cardiac malformations may be present such as cleft palates. Most cases result in stillbirth or death shortly after birth. Depending on the position of the heart from birth ectopia cordis can be classified into four categories namely - cervical, thoracic, thoracoabdominal and abdominal.
- Malposition (Dextrocardia)
- Dextrocardia is the presence of the heart ion the right hemithorax with the apex of the heart points to the right side of the chest. It is usually associated with major anomalies of the heart e.g. transposition of the atria or great arteries.
-
Course dashboard
Click here to access Unit one Content..
Topic 2.4: SHUNTS (CYANOTIC CONGENITAL HEART DISEASES)
- INTRODUCTION
- A shunt is an abnormal communication between heart chambers, between blood vessels or between the heart chambers and blood vessels. The pressure differences in heart chambers determines the direction of shunting of the blood - left-to-right shunting (more common) or right-to-left shunting.
- CLASSIFICATION
- Left-to-right shunts (late cyanosis or acyanotic heart diseases)
- Atrial Septal Defect (ASD)
- Ventricular Septal Defect (VSD)
- Patent Ductus Arteriosus (PDA)
- Atrioventricular Septal Defect (AVSD)
- Right-to-left shunts (early cyanosis or cyanotic heart diseases ) – 5TS
- Tetralogy of Fallot (TOF)
- Transposition of great arteries
- Truncus arteriosus and stenosis
- Tricuspid atresia and stenosis
- Total anomaly of pulmonary venous drainage/connection
Course dashboardClick here to access Unit one Content..
Topic 2.5: LEFT-TO-RIGHT SHUNTS (Acyanotic Heart Disease)
- These cause cyanosis several months or
years after birth.
- Atrial Septal Defect (ASD)
- Description
- ASD is an abnormal opening in the atrial septum that allows free communication between the left and right atria. It accounts for 10% of congenital heart diseases. It is usually asymptomatic until in the adulthood when pulmonary hypertension (in 10% cases) is induced causing late cyanotic heart disease and right-sided heart failure.
- The effects are produced due to left-to-right shunt at the atrial level with increased pulmonary flow. These result in hypertrophy of the right atrium and ventricle, enlargement and haemodynamic changes in tricuspid and pulmonary valves, reduction in size of left atrium and left ventricle and reduction in size of the mitral and aortic orifices.
- Features
- Right ventricular hypertrophy
- Cardiac failure
- Cyanosis (late)
- Haemodynamic changes + Murmur
- Failure to thrive
Review Questions
- Explain the pathophysiology of these features.
- How will use elicit them on physical examination
Course dashboardClick here to access Unit one Content..
Topic 2.6: LEFT-TO-RIGHT SHUNTS (Acyanotic Heart Disease) Cont'd
Ventricular Septal Defect (VSD)
- VSD is the most common congenital anomaly of the heart in which there is incomplete closure of the ventricular septum allowing free communication between the left and right ventricles. VSD is usually recognized early in life. 30% cases occur in isolation but it is frequently associated with other structural anomalies especially the Tetralogy of Fallot. 50% of the smaller defects of less than 0.5 cm in diameter close spontaneously. The clinical features range from asymptomatic murmurs to late cyanosis and fulminant chronic heart failure depending on the size of the defect.
- The effects are produced due to left-to-right shunt at the ventricular level, increased pulmonary flow and increased volume in the left side of the heart. These result in hypertrophy and dilatation of the right atrium and ventricle, endocardial hypertrophy of the right ventricle and enlargement and haemodynamic changes in all the heart valves
- Features
- Hypertrophy and dilatation of the right atrium
- Hypertrophy and dilatation of the right ventricle
- Murmur
- Cardiac failure
- Failure to thrive
- Patent/Persistent Ductus Arteriosus (PDA)
- The ductus arteriosus (DA) is a normal vascular connection between the aorta and the bifuractaion of the pulmonary artery which allows communication between the aorta and the pulmonary artery in the foetus (foetal life). Normally at term the ductus closes within the first 1-2 days of life as a result of muscular contraction due to the effect of relatively high oxygen tension and reduced local prostaglandin E (PGE2) synthesis. Persistence of ductus arteriosus beyond 3 months of life is usually permanent and abnormal.
- PDA which accounts for 10% of congenital heart diseases usually occurs as an isolated anomaly in 85-90% cases. It may be associated with VSD, coarctication of the aorta and pulmonary or aortic stenosis. There is an accompanying left ventricular hypertrophy and pulmonary artery dilatation.
- The cause for patency of the DA is idiopathic but it is associated with continued synthesis of PGE2 after birth. This has been established by evidence of association of respiratory distress syndrome (RDS) with PDA and pharmacologic closure of PDA with administration of indomethacin to suppress PGE2 synthesis
- Effects
- Loud murmur (machinery murmur)
- Pulmonary hypertension
- Right ventricular hypertrophy
- Right atrial hypertrophy
- Dilated ascending aorta
Course dashboardClick here to access Unit one Content..
Topic 2.7: RIGHT-TO-LEFT SHUNTS (Cyanotic Congenital Heart Disease)
- In right-to-left shunts there is shunting
of blood from the right side of the heart to the left side allowing entry of
poorly oxygenated blood into the systemic circulation. This results in early
cyanosis hence the description of congenital cyanotic heart disease. These
shunts (communication channel) can allow movement of emboli from venous sources
to pass directly into the systemic circulation resulting in what we would call paradoxical
emboli.
- Tetralogy of Fallot (TOF)
- TOF accounts for 10% of children born with heart abnormalities. It is composed of four (tetralogy) cardinal anomalies namely: -
- VSD (the shunt)
- Displacement of the aorta to the right side (dextraposition of the aorta) so as it overrides the VSD
- Pulmonary stenosis (obstruction) with ventricular outflow obstruction
- Right ventricular hypertrophy
- Severity of symptoms in TOF is determined by the extent of right ventricular outflow obstruction and the size of the VSD. A large VSD and a mild pulmonary stenosis lead to a left-to-right shunt without cyanosis and a severe pulmonary stenosis results in a cyanotic right-to-left shunt. When there is complete obstruction survival can only occur through a patent ductus arteriosus (PDA) or dilated bronchial arteries.
- Effects
- Hypertrophy of the right atrium and right ventricle
- Cyanosis
- Failure thrive
- Cardiac failure
Transposition of Great Arteries (TGA)
This describes malformations with regard to the position of the aorta, pulmonary trunk, atrioventricular orifices and the position of the atria in relation to ventricles. The aorta arises from the right ventricle and the pulmonary artery emanates from the left ventricle. TGA is common in children of diabetic mothers. The 2 common types are regular transposition (commonest type) and corrected transposition. In regular transposition the aorta is displaced anteriorly and the to the right of the pulmonary trunk
During the foetal life, development proceeds as there is mixing of venous and systemic blood thorough the PDA and a patent foramen ovale. Postnatally, life will depend on continued patency of PDA, presence of VSD, ASD or a patent foramen ovale. In majority of the cases children die within the first few weeks/months if untreated and the prognosis depends on severity of tissues hypoxia and the ability of the right ventricle to maintain aortic blood flow.
Course dashboardClick here to access Unit one Content..
Topic 2.8: RIGHT-TO-LEFT SHUNTS (Cyanotic Congenital Heart Disease) Cont'd
- Truncus Arteriosus
- This is a rare abnormality with a poor prognosis associated with numerous connected defects of the heart. The embryological structure known as the truncus arteriosus never properly divides into the pulmonary artery and aorta resulting in a single large common vessel receiving blood from both the left and right ventricle. There is an associated VSD. The patient presents with early cyanosis due to the right-to-left shunt but the flow later reverses and the patient develops right ventricular hypertrophy with pulmonary vascular hypertension.
Classification
- Type I: truncus -> one pulmonary artery -> two lateral pulmonary arteries
- Type II: truncus -> two posterior/posterolateral pulmonary arteries
- Type III: truncus -> two lateral pulmonary arteries
- Clinical Features
- Heart failure occurs within weeks
- Systolic ejection murmur is heard at the left sternal border
- Widened pulse pressure
- Bounding arterial pulses
- Loud second heart sound
- Biventricular hypertrophy
- Cardiomegaly
- Increased pulmonary vascularity
- Tricuspid Atresia and Stenosis
- Is an abnormality often associated with pulmonary stenosis and atresia with an inter-atrial defect through which right-to-left shunting of blood occurs. There is absence of tricuspid orifice in tricuspid atresia and a small tricuspid ring with malformed valve cusps in tricuspid stenosis. Children with tricuspid atresia are cyanotic since birth and live for a few weeks or months.
- Features
- Progressive cyanosis
- Poor feeding
- Tachypnea over the first 2 weeks of life
- Holosystolic murmur due to the VSD
- Left axis deviation on electrocardiography and left ventricular hypertrophy (since it must pump blood to both the pulmonary and systemic systems)
- Total Anomaly of the Pulmonary Venous Drainage (TAPVD)
- TAPVD is a rare cyanotic congenital heart defect (CHD) in which all four pulmonary veins are malpositioned and make anomalous connections to the systemic venous circulation. There are no pulmonary veins directly joining the left atrium hence drainage is into the left innominate vein or to the coronary sinus.
- Normally, pulmonary venous return carries oxygenated blood to the left atrium and to the rest of the body. A patent foramen ovale or an atrial septal defect must be present, or else the condition is fatal due to a lack of systemic blood flow. PDA or a ASD is normally present and allows pulmonary venous blood to enter the left atrium.
- Features
- Volume and pressure hypertrophy of the right atrium and right ventricle
- Cyanosis
- Murmur (systolic ejection)
- Right ventricular heave
- Right ventricular hypertrophy
- Cardiac failure
- Cardiomegaly
- Splitting of S2
- S3 gallop
- Failure to thrive
- Cyanosis, tachypnea, dyspnoea since the overloaded pulmonary circuit can cause pulmonary edema
Course dashboardClick here to access Unit one Content..
Topic 2.9: OBSTRUCTIVE CONGENITAL ANOMALIES
- They result in obstruction to blood flow
from the heart and are classified as obstruction in the aorta e.g.
coarctication of the aorta, obstruction to outflow from the left ventricle –
aortic stenosis and atresia and obstruction to outflow from the right ventricle
– pulmonary stenosis and atresia
- Coarctication of the Aorta
- The aorta is compressed or contracted and 50% cases occur as isolated defects with the remaining occurring with multiple other anomalies of the heart. There is localized narrowing of the aorta in any part with the constriction being more often distal to the ductus arteriosus (post-ductal or adult type) or occasionally proximal to the ductus arteriosus (pre-ductal or infantile type) on the transverse aorta. Causes of Death: Chronic cardiac failure, aortic dissection, intracranial haemorrhage and infective endocarditis
- The most common abnormality of the aorta is bicuspid aortic valve, which has less functional significance but predisposes to calcification. Complete aortic atresia is rare and incompatible with neonatal survival. Aortic stenosis may be congenital or acquired.
- Congenital aortic stenosis is of three types –
- Valvular stenosis where there valves cusps are irregularly thickened and malformed
- Subvalvular where there is a thick fibrous ring under the aortic valves causing subaoratic obstruction and
- Supravalvular stenosis that has a fibrous constriction above the sinuses of valsalva.
- Effects
- Left ventricular hypertrophy (pressure overload)
- Post-stenotic dilatation of the aortic root
- Infective endocarditis
- Sudden death (rare)
- Pulmonary Stenosis and Atresia
- This is the commonest form of obstructive congenital heart disease where there is fusion of the cusps of the pulmonary valve forming a diaphragm like obstruction to blood flow and it may also occur as a component of TOF or may occur in conjunction with transposition abnormalities. In pulmonary stenosis there is no communication between right ventricle and the lungs so blood bypasses the right ventricle through an inter-atrial septal defect and enters the lungs via the PDA. WHAT ARE THE FEATURES?
Course dashboardClick here to access Unit one Content..
Topic 2: Further Reading
- Kishasha M (2016). Textbook of human pathology. 1st edition, Acrodile publishers, Nairobi, Kenya.
- Harsh M (2014). Textbook of Pathology. 1st edition. New Delhi: Jaypee Brothers, Medical Pub, India
- Ngton C, & Muir (2014). Textbook of Pathology. 15th edition, New Delhi. Jaypee Brothers, India
Course dashboardClick here to access Unit one Content..
Topic 3.1: Cardiac Failure (Heart Failure)
- Learning Outcomes
- At the end of the lesson the learner should be able to: -
- Define cardiac failure
- Explain the pathophysiologic mechanisms of cardiac failure
- Describe the adaptive mechanisms in cardiac failure
- Describe the causes of cardiac failure
- Describe the pathology of cardiac failure with respect to each cause
Course dashboardClick here to access Unit one Content..
Topic 3.2: INTRODUCTION AND DEFINITION
- Cardiac failure is a situation when the ventricular myocardium fails to maintain a circulation adequate for body requirements despite adequate venous return. The heart is unable to deliver a supply of oxygenated blood that is adequate for meeting metabolic needs of peripheral tissues both at rest and during exercise. It can be viewed as a condition when the output of the heart is insufficient for the needs of the body tissues. Physiologically heart failure is a state in which an increase in filling pressure and therefore fibre length causes a fall rather than a rise n cardiac output.
- PATHOPHYSIOLOGIC AND COMPENSATORY MECHANISMS
- Heart Function
- The functioning of the heart is guided by intimate integrating four principle determinants that regulate the stroke volume and cardiac output. There are two intrinsic factors - preload (ventricular end-diastolic volume) and afterload (intraventricular systolic tension during ejection) and two extrinsic autonomic modulations - contractility (variable force of ventricular contraction independent of loading) and heart rate (frequency of contraction).
- During normal life the heart faces variable workload hence the need for the adaptive physiologic mechanisms that assist it in meeting the increased demands and adaptive mechanisms enable the heart to handle the extraordinary loads that may be placed on it by such conditions as diseased valves or poor myocardial function.
- The Basic Adaptive Mechanisms
- The cardiovascular system maintains arterial pressure and perfusion of vital organs when there is huge haemodynamic burden or disturbance in myocardial contractility through a number of adaptive mechanisms geared to sustaining adequate cardiac performance. These adaptive mechanisms include – Frank-Starling Mechanism, Myocardial Structural Changes and Activation of neurohormonal systems.
- Frank-Starling Principle
- In a normal heart the resting or diastolic muscle length is determined by the end-diastolic volume (EDV), which is closely related to the end diastolic pressure (EDP). Increased preload of dilatation increases cross-bridges in the sarcomeres and the tension or pressure generated enhances muscle contraction during systole hence an increase in stroke volume and cardiac output. Thus an increase in left ventricular end-diastolic volume or pressure causes an increase in stroke output or work.
- Myocardial Structural Changes
- Cardiac Hypertrophy
- Hypertrophy entails an increase both in the size of individual muscle cells and in the overall muscle mass due to increased myofibrils, mitochondria and size of myocytes. It results from chronic pressure overload and helps the heart overcome pressure load. It has limitations in that a hypertrophied muscle operates at a lower inotropic state than the normal heart muscle. Increased fibrous tissue and muscle causes decreased compliance (poor filling) and increased oxygen demand (causes subendocardial ischaemia).
- Cardiac Dilatation
- Dilatation is a late adaptive mechanism in which the stroke volume increases resulting in dilatation of the ventricle due to volume overload as in aortic regurgitation or mitral regurgitation. Within certain limits ventricular dilatation effects compensatory increase in cardiac output by the Frank-Starling mechanism.
- Dilatation in the absence of a volume overload is an indication of ventricular failure. An increase in the ventricular radius causes an increase in wall tension with a concomitant increase in energy needs (increased oxygen consumption) and a decline in efficiency of contraction.
- Activation of Neurohormonal Systems
- Norepnephrine
- Release of norepinephrine by adrenergic cardiac nerves increases heart rate and augments myocardial contraction.
- Heart Rate
- In an individual with a normal heart changes in heart rate do not affect cardiac output significantly because compensatory changes in stroke volume occur to offset the alterations in rate. At slower heart rates, the stroke volume increases because there is prolonged left ventricular filling while at faster heart rates ventricular filling time decreases and the stroke volume declines.
- Contractility
- The tension developed by a contracting heart muscle is related to the inotropic state of the cardiac muscle which is the velocity with which the muscle contracts. At a higher inotropic state (increased contractility), the muscle contracts faster for any given load and develops more tension.
- Sympathetic nervous activity, circulating catecholamines and digitalis increase contractility of the heart muscle while cardiomyopathy, hypertrophy and ischaemia reduce contractility. There are changes in end-diastolic volume and in the inotropic state to achieve alterations of cardiac output. Increased contractility increases wall tension and oxygen demand.
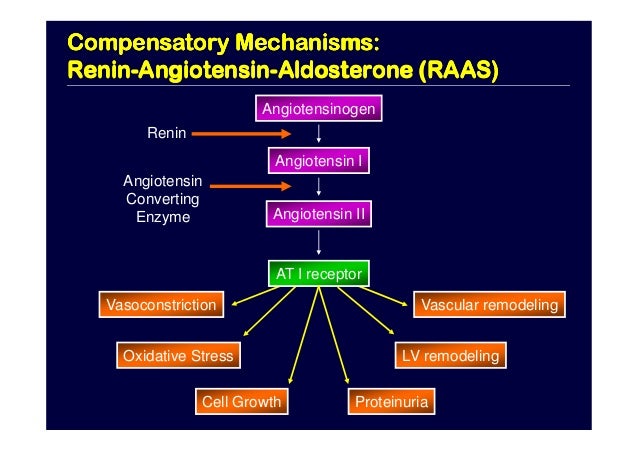
- Activation of Renin-Angiotensin Aldosterone (RAA) System
- This results in retention of fluid and increased peripheral resistance leading to increased cardiac output and increase in blood pressure.
- Release of Atrial Natriuretic Peptide (ANP)
Course dashboardClick here to access Unit one Content..
Topic 3.3: COMPENSATORY ENLARGEMENT OF THE HEART
- Introduction
- Compensatory enlargement of the heart prevents heart failure or postpones heart failure. This is achieved through three processes namely: - hypertrophy (results from increased demand for pumping) dilatation (accommodation of Excessive blood) and remodelling (change in structure of myocytes)
- The cardiac reserve represents the activity of the heart to meet increased demands and thus the heart is able to adjust its output by changes in rate and increased stroke volume (main advantage). When the primary cardiac compensation fails, extra cardiac mechanisms may assist and these include - increased blood volume through retention Na+/H20 and decreased renal blood flow; redistribution of volume, haematologic adjustments decreased blood flow causing marrow anoxia (organ/tissues) resulting in increased red blood cell production and increased oxygen extraction by tissues.

- Classification
- The compensatory changes in heart failure can be classified as: -
- Local
- Chamber enlargement
- Myocardial hypertrophy
- Increased heart rate
- Systemic Changes
- Activation of the sympathetic nervous system
- Activation of RAAS
- Release of ANP
- Release of ADH
- Why do these compensatory mechanisms can fail?
- These may be due to altered venous return (alterations) - deficient return or too much (overload); increased resistance to flow and impaired cardiac Contraction
Course dashboardClick here to access Unit one Content..
Topic 3.4: CAUSES OF CARDIAC ENLARGEMENT
- Enlargement of the heart occurs due to increased workload (volume and pressure).
- 1. Left Ventricular Hypertrophy (LVH)
- Common causes of marked left ventricular hypertrophy include: -
- Systemic Hypertension
- Aortic stenosis and regurgitation or mitral regurgitation
- Mitral insufficiency
- Coartication of the Aorta
- Collusive coronary artery disease
- Congenital abnormalities e.g. septal defects - PDA
- High Cardiac output states- thyrotoxicosis, severe anaemia and A – V fistula
- Mild left ventricular hypertrophy is caused by hypertrophic cardiomyopathies and left ventricular failure of any cause
- 2. Right Ventricular Hypertrophy (RVH)
- Left ventricular hypertrophy (LVH)
- Chronic Lung disease – e.g. chronic emphysema, bronchioectasis, pneumoconiosis, pulmonary vascular disease
- Pulmonary stenosis and insufficiency
- MitraI regurgitation (MR), Mitral Stenosis (MS)
- Congenital heart disease (C.H.D) with shunts
- Pulmonary stenosis (PS)
- LVH/LVF
- 3. Compensatory Dilatation
- Follows valve incompetence or shuts and is usually accompanied by hypertrophy of the respective ventricles.
- Causes
- Valvular insufficiency – mitral and/or aortic regurgitation in Left ventricular dilatation and tricuspid and/or pulmonary regurgitation in right ventricular dilatation.
- Left-to-right shunts e.g. VSD
- Conditions with high output states – give examples
- Myocardial diseases e.g. cardiomyopathy (which type?)
- Systemic hypertension
Course dashboardClick here to access Unit one Content..
Topic 3.5: CAUSES OF CARDIAC FAILURE
- The causes of cardiac failure include: -
- Intrinsic pump failure
- Increased work load on the heart - Pressure overload and Volume overload
- Impaired filling of the cardiac chambers
- Multifactorial ( a combination of the above factors)
- PUMP FAILURE
- Introduction
- Intrinsic pump failure is the most common and important cause of heart failure. The heart has 2 main pumps: - the left pump which pumps blood to the peripheral organs and the right one that pumps blood to the lungs. Pump failure frequently results from weakness of ventricular contractions.
- Causes of Intrinsic Pump Failure
- Myocardial weakness
- Cardiac rhythm disorders
- Reduced or poor myocardial response
- Multifactorial (multiple causes)
- MYOCARDIAL WEAKNESS
- Introduction
- A situation where muscle weakness leads to unsatisfactory pumping action of the heart muscles due to reduced contractibility of myocardium leading to secondary reduction of Blood supply.
- Causes
- The causes of myocardial weakness can classified based on aetiology or function.
- Aetiological Classification
- Myocardial Ischaemia and infarction – results from reduced blood supply e.g. in coronary artery diseases due to atherosclerosis, thrombo-embolism, and haemorrhage into the intima, vasculitis, external pressure and muscular spasm of vessel wall.
- Infections
- Viral myocarditis - Coxsackie A, B, Echo, Rubella
- Bacterial toxins - infective endocarditis, Diphtheria [Bacillus] – causes peripheral circulatory failure and toxic myocarditis causing AV/BB Block, staphylococcus and streptococcus
- Fungal/Parasitic – actinomycosis, toxoplamsosis, histoplasmosis, aspergillus and Filariasis (Loa loa)
- Protozoal - Cruz trypanosomiasis (Chagas Disease)
- Nutritional Deficiency states- Beri Beri (Thiamine) - Thiamine is used as a co-enzyme Carbohydrate metabolism and for synthesis of acetylcholine. It’s deficiency causes fatty degeneration of the heart muscles and reduced nerve impulse conduction.
- Systemic connective Tissue Disorders - rheumatoid arthritis, systemic lupus erthromatosus (S.L.E) and polyarteritis Nodosa.
- Cardiomyopathies - reduces the contractibility of the myocardium
- Metabolic/Endocrine - diabetes mellitus, altered Thyroid function [Hyperthyroidism/Hypothyroidism], adrenal cortical insufficiency and acromegaly.
- Storage disorders - Glycogen storage disease
- Infiltrations – Amyloidosis, Sarcoidosis, Heamochromatosis
- Sensitivity and Toxic reactions - drugs e.g. cytotoxic drugs, alcohol, cobalt and barbiturates
- Physical agents - Irradiation
- Functional Classification
- This is based on whether the chambers are dilated or not. Dilatation can be generalized or focal. Myocardial weakness may be due to hypertrophic and/or restrictive cardiomyopathy
- Pathology of Myocardial Weakness
- Expulsion of blood by the ventricles during systole is reduced due to the weak pumping action of the ventricles leaving a residual blood volume.
- During diastole the chambers dilate to contain both residual and incoming blood causing dilatation of the ventricles putting the ventricles at a greater disadvantage as more force will be required to pump out the increased volume of blood (Frank-Starling Law). But due to the weakness of the myocardium, this is will not achieved and therefore blood pools in the ventricles.
- If the destruction is not halted, dilatation of the ventricles and failure are progressive.
- Ventricular dilation (left ventricle and right ventricle) leads to the stretching of the respective valves (mitral and tricuspid) resulting in valve incompetence of the Mitral and Tricuspid valves respectively.
- This worsens the situation due to reduced cardiac output and damming of blood in veins which increase systemic venous pressure (systemic venous pressure) slowing the general circulation.
Course dashboardClick here to access Unit one Content..
Topic 3.6: CARDIAC RHYTHM DISORDERS
- Effective pumping action of the heart is
achieved by alternate relaxation and contraction allowing blood to enter the
chambers (during relaxation – diastole) and force in out during contraction
(systole). This is achieved by the co-ordination, conduction and rhythmicity of
the cardiac muscle together with the efficiency of the conducting system of the
heart, which comprises of the sino atrial Node (SAN), atrial Ventricular Node
(AVN), the Purkinje tissue and the Bundle of His.
- Circus Movement
- The cardiac impulse conduction around the heart without stopping hence there is continuous impulse conduction due to an enlarged heart (long pathway), slow conduction e.g. failure of the purkinje tissue, decreased refractory period which results from epinephrine, sympathetic stimulation and irritation of the heart by disease and transmission of impulses in figures of 8’s for example in ventricular fibrillation
- Rhythm Disorders
- Arrhythmias can be can disorders of impulse conduction at sites such as the SAN, AVN, atria, Ventricles and Purkinje tissues or disorders of impulse formation in the form of abnormal site of origin or abnormal rate of impulse discharge.
- Tachycardia
- This is a rhythm rate greater than 100 beats per minute. Causes of tachycardia include: exercise, anxiety and any disorder that increases the sympathetic nervous system stimulation
- Pathology
- Tachycardia impairs diastolic refilling of ventricles and shortens the coronary artery diastolic filling reducing blood supply to the heart. This results in decreased stroke volume and cardiac output thus decreasing blood supply to the myocardium resulting in ischaemia [Myocardial], which reduces the performance of the heart. Examples of Tachycardia are: - atrial fibrillation, atrial flutter, paroxysmal Tachycardia and atrial tachycardia
- Atrial fibrillation
- Atrial fibrillation is an impulse transmission of 350 – 600 beats per minute. The impulse is irregular in time and force. It is worse on exercise.
- Pathology
- Fewer impulses reach the ventricles to effect contraction and therefore the stroke volume and cardiac output reduce hence compromising blood supply and there is irregular ventricular response to transmission of impulses from the atria. The resulting incompetent emptying of the ventricles causes pooling of blood in the heart chambers leading to dilatation and hypertrophy of the ventricles and cardiac failure if the situation is not reversed
- Causes
- Rheumatic Heart Disease (RHD), coronary Heart disease, hypertensive heart disease. Thyrotoxicosis, cardiomyopathies (Dilated and hypertrophic cardiomyopathy), constrictive pericarditis, pulmonary embolism and alcohol abuse
- Atrial Flutter
- Atrial flutter is an impulse frequency of 125– 300 beats per minute. It is usually regular but can become irregular if there is fluctuating heart block.
- Pathology
- Fewer impulses reach the ventricles to effect contraction and therefore the stroke volume and cardiac output are reduced hence compromising blood supply. There is irregular ventricular response and the resulting incompetent emptying of the ventricles causes pooling of blood in the heart chambers leading to Dilatation and
- Causes
- Digoxin toxicity, cardiomyopathy, chronic ischaemic heart disease and rheumatic heart Disease (RHD)
- Paroxysmal Tachycardia
- Is an impulse transmission of 150 – 250 beats per minute and it is intermittent
- Bradycardia
- Bradycardia is an impulse rate of below 60 beats per minute
- Pathology
- In partial heart block at SAN some impulses reach ventricles to effect contraction but stroke volume cardiac output and heart rate are reduced but in total heart block at SAN no impulses pass to effect ventricular contraction hence the ventricles contract at 25 beats/min. (Normal for ventricular Tissue). This is inadequate to sustain required blood supply.
- Causes
- Physiological (athletes and during sleep) and pathological - cardiac - acute Myocardial infarction, drugs (Beta blockers, Digoxin) and heart block; non cardiac - hypothyroidism, obstructive jaundice and increased intracranial pressure
- Heart Block
- Interferes with the conduction process and impulses are blocked from getting through the ventricular myocardium resulting in ventricles contracting at a much slower rate than normal. This can occur at the SAN, AV – Block; 1st degree there is delayed impulse transmission from to ventricles; 2nd degree there is intermittent failure of impulse transmission (Mobitz I block, Mobitz II block and 2:1 or 3:1 (advanced) block and 3rd degree where there is complete A–V block
- Causes
- Myocardial infarction, digoxin toxicity, idiopathic fibrosis, congenital heart disease, aortic valve disease, infiltration - tumours, syphilis, endocarditis, inflammation - rheumatoid arthritis, ankylosing spondylitis, Reiter’s syndrome and sarcoidosis, rheumatic fever and diphtheria
Course dashboardClick here to access Unit one Content..
Topic 3.7: INCREASED WORKLOAD ON THE HEART
- PRESSURE OVERLOAD
- This is a situation where there is increased resistance to the expulsion of blood from the ventricles or inflow of blood into ventricles.
- Causes
- Left Ventricle - aortic stenosis and systemic hypertension
- Right ventricles - pulmonary hypertension, mitral stenosis and lung Disease
- Pathology
- This can be considered in two groups of ventricular outflow obstruction and ventricular inflow obstruction.
- Ventricular Outflow Obstruction
- This can be as a result of hypertension (pulmonary and systemic hypertension), aortic stenosis and pulmonary Stenosis
- Pathology
- Obstruction to out flow of blood from the ventricles causes increased afterload (ventricular) with the response of ventricular hypertrophy but the ventricular capacity remains (Starling’s Law)
- Increased in ventricular muscle bulk causes muscles stiff and this will require higher atrial pressure for refilling and so there occurs Atrial hypertrophy
- With the increased load due to increased afterload the ventricles dilate needing high wall tension to maintain the systolic pressure (Laplace’s Law)
- Coronary vessels are unable to supply the increased muscle bulk with adequate blood so the muscle fibres become ischaemic and die off. The ischaemic muscle tissue is replaced by fibrous tissue, which has poor contractibility.
- Ventricular Inflow Obstruction
- Causes
- This can result from mitral stenosis, tricuspid stenosis, cardiac tumours, external Pressure or Constriction e.g. constrictive pericarditis and endomyocardial fibrosis
- Pathology
- Obstruction of in flow of blood from the atria causes increased afterload (atrial) with the response of atrial hypertrophy but the atrial capacity remains (Starling’s Law)
- Increase in atrial muscle bulk makes them stiff and this will require higher systemic venous pressure for refilling and emptying and so there occurs atrial hypertrophy
- With increased load (due to increased afterload) the atrial dilatation requires high wall tension to maintain the systolic pressure (Laplace’s Law) hence there occurs pooling of blood in the systemic and pulmonary vessels. This reduced ventricular filing
- Reduced ventricular filling cardiac output is reduced
- Coronary vessels are unable to supply the increased muscle bulk with adequate blood so the muscle fibres become ischaemic and die off. The ischaemic muscle tissue is replaced by fibrous tissue, which has poor contractibility
- The increased atrial action causes hypertrophy and dilatation, which result in Atrial fibrillation
- VOLUME OVERLOAD
- This occurs when the ventricles are required to expel more than the normal amount of blood
- Causes
- Incompetent valves that allow blood to flow back into the chambers increasing the blood volume e.g. aortic regurgitation and pulmonary regurgitation.
- States with high general circulation (High Output States) such as severe anaemia, thyrotoxicosis, Beriberi and patent Ductus Arterious (PDA).
- Hypoxia resulting from lung disease (increase circulation) e.g. cor pulmonalae which leads to an increase in circulation.
- Arterio-venous shunts between the left and right sides of the circulation causing cyanosis and hence hypoxia which causes increased circulation
- Explanation/Pathology
- The pathology is based on the effects of ventricular hypertrophy and dilatation, Frank-Starling’s Law and Laplace’s Law
- IMPAIRED FILLING OF THE CARDIAC CHAMBERS
- The cardiac output is decreased and cardiac failure ensues due to extra cardiac causes or defects in the filling of the heart chambers as seen in cardiac tamponade and constrictive pericarditis
- MULTIPLE FACTORS
- This involves a combination of the above-mentioned factors.
Course dashboardClick here to access Unit one Content..
Topic 3: Further Reading
Kishasha M (2016). Textbook of human pathology. 1st edition, Acrodile publishers, Nairobi, Kenya.
Harsh M (2014). Textbook of Pathology. 1st edition. New Delhi: Jaypee Brothers, Medical Pub, India
Ngton C, & Muir (2014). Textbook of Pathology. 15th edition, New Delhi. Jaypee Brothers, India
Course dashboardClick here to access Unit one Content..
Topic 4.1: Manifestations of Cardiac Failure
-
- Learning Outcomes
- At the end of the lesson the learner should be able to: -
- Describe the pathophysiology of features of cardiac failure
- Describe the cardinal features of cardiac failure
- Relate between left ventricular failure (LVF) and right ventricular failure (RVF).
- Explain the effects of cardiac failure on other body organs
- Investigate cardiac failure
- Interpret results of various investigations
Course dashboardClick here to access Unit one Content..
Topic 4.2: INTRODUCTION
- Important factors that determine performance of the heart are the venous return, resistance to outflow, contractibility and heart rate. These factors depend on coronary blood flow(which is 40% of cardiac output and delivers 70% oxygen for the heart function) pressure gradient (and extravascular compression of the aortic pressure) and regulation : - autoregulation – vasodilatation metabolites increase when myocardial PC02 increase and PO2 reduces, metabolic regulation – main controlling factor and neurohormonal control (hormones and ANS)
- CLASSIFICATION
- Manifestations of cardiac failure depend on the rate of development of the casual factors and the side of the heart affected. Development of causal factors can results in acute or chronic cardiac failure. The side of the heart involved that is left side (Left ventricular failure - LVF), right side (Right Ventricular Failure - RVF) and total heart failure (congestive cardiac failure) when both sides of the heart are [Congestive cardiac failure - CCF (LVF + RVF)]
-
-
Grading Of Cardiac Failure - New York Heart association (NYHA) Classification
Grade I Exercise tolerance is uncompromised
Grade II Exercise tolerance is slightly compromised
Grade III Exercise tolerance is moderately compromised
Grade IV Exercise tolerance is severely compromised
ACUTE CARDIAC FAILURE
- Causal factors develop rapidly or suddenly as in myocardial infarction (massive), gross pulmonary embolism, cardiac arrhythmias, acute bacterial toxaemia, rheumatic fever and rapture of Ventricles and valve cusps. In severe cases of acute cardiac failure (due to myocardial infarction) there is marked reduction in cardiac output with selective peripheral vasoconstriction following sympathetic activity causes CARDIOGENIC SHOCK with central venous pressure increased (different for Hypovolaemic shock and hence the different principles of management). There is decreased cardiac output that leads to cerebral hypoxia
- CHRONIC HEART FAILURE
- The causal factors develop gradually (slowly) as in myocardial ischaemia due to artheroma, severe systemic hypertension, chronic valvular disease/lesions and chronic lung disease causing hypoxia leading to Pulmonary Hypertension. In this regard cardiac output is diminished and tissue hypoxia results.
Course dashboardClick here to access Unit one Content..
Topic 4.3: LEFT SIDED HEART FAILURE (LEFT VENTRICULAR FAILURE, LVF)
- Introduction
- The left ventricle is more commonly affected than the right ventricle. Left ventricular failure leads to right ventricular failure then total heart failure (CCF).
- Causes of LVF
- Ischaemic Heart Disease (IHD) particularly Myocardial Infarction
- Chronic Hypertension/Hypertension
- Aortic valvular disease due to rheumatic endocarditis, aortic stenosis (calcific), syphilitic heart disease and congenital heart disease
- Mitral incompetence/mitral valve disease
- High output conditions such as anaemia, valve regurgitation, fever, thyrotoxicosis, atrio-ventricular malformations, Beri Beri and Paget’s disease of bones
- Cardiomyopathy
- Adhesive mediastino-pericarditis
- Pathology
- During systole the left ventricle fails to expel all the blood it receives hence contains an increasing volume of blood at the end of systole
- During the next diastole there is accumulation of the residual blood (left during systole) and the incoming blood during diastole. Increased diastolic volume causes dilatation of the ventricle further increasing inadequacy of contraction.
- Ventricular dilation causes stretching of valve rings (mitral 10cm) resulting in incompetence (Mitral Regurgitation - MR)
- Mitral regurgitation allows some blood expelled during systole passes through the valve to the left atria increasing pressure here (left atria) causing venous congestion in the pulmonary system causing oedema of the lungs (pulmonary oedema)
- Pulmonary congestion leads to shortness of breath, orthopnoea, PND and haemoptysis.
- This retrograde loss of blood through the leaking valve further compromises the ventricular output and cardiac output.
- Decreased output causes renal ischaemia (acute tubular necrosis, oliguria), CNS ischaemia -anoxic neuronal changes (dizziness, confusion), bowel ischaemia – mucosal or transmural necrosis (GI bleeing, sepsis) and skeletal ischaemia (weakness, fatigue, reduced exercise tolerance)
- With the situation persisting there is ventricular dilatation and hypertrophy.
- Clinical Features (Manifestation)
- The clinical manifestations result from insufficient blood flow through the various body organs and tissues plus the pulmonary congestion due to stasis of blood in the pulmonary circulation. The clinical manifestations include or involve the heart (size, abnormal heart sounds, pulse), the lungs (dyspnoea, orthopnoea, paroxysmal nocturnal dysnpoea (PND), cough, and cyanosis), pedal oedema, kidneys, brain and the liver
- The Heart
- Size – cardiomegally
- Abnormal heart sounds
- The Pulse rate – there can be tachycardia or bradycardia
- Pulse rhythm and pulse character
- Cardiomegally
- There is an increase in the heart side due to dilatation and hypertrophy of the heart chambers. Assessment of cardiomegally is based on subjective visual impression, physical examination (palpation of the apex beat), determination of the cardio-thoracic ratio and volume measurement (length x width x depth x 0.63)
- Abnormal Heart Sounds
- There may be a third or fourth heart sound. The third Heart sound (S3 Gallop) occurs due to rapid ventricular filling. This can be due to young age (normal), constrictive pericarditis, rheumatic mitral stenosis, severe non-rheumatic mitral regurgitation and valvular heart disease – mitral/Aortic regurgitation. The fourth heart sound (S4 Gallop) occurs in situations of increased atrial activity due to left ventricular disease, left ventricular hypertrophy, dilated heart cavity, pulmonary stenosis, pulmonary hypertension and acute myocardial infarction
- The Pulse
- Pulsus paradoxicus (Kussmal’s sign) or Pulsus alternans
- The Lungs
- The effects seen in the lungs are dyspnoea, cyanosis, cough and crepitations. Congestion and oedema occur in the pulmonary venous circulation and the alveolar capillaries as the fluid collects in alveoli (pulmonary) and in severe cases rhexis of red blood cells into the capillaries occurs causing haemorrhage into alveolar spaces. Dyspnoea occurs due to inadequate oxygenation of blood flowing though functionally impaired lungs. anoxaemia of respiratory centre and the carotid sinus and decreased vital capacity of lungs due to vascular distension
- PND (Paroxysmal Nocturnal Dyspnoea)
- Pulmonary congestion and oedema are worsened by severe functional imbalance of ventricles
- Excessive sympathetic activity causes venoconstriction so blood moves from the systemic veins to the pulmonary circulation.
- During sleep, irritability of CNS decreases hence accumulation of oedema with provoking defence system e.g. cough
- Decreased muscular activity allows pooling of blood in veins and change in position or movement expels blood causing sudden increase volume in the lungs.
- Reabsorption of interstitial fluid in recumbence causing increase blood volume.
- In active state, hydrostatic pressure at the capillary level is high leading to fluid effusion into the interstitial spaces. At night (inactive) the reverse happens leading to net fluid flow in the vascular system, heart and pulmonary circulation leading to congestion causing paroxysmal dyspnoea
- The patient lying down improves the venous return from the limbs worsening the situation.
- Cough occurs as a result of irritation of mucosa (oedema fluid). The cough may be productive of blood-streaked, frothy sputum due to pulmonary congestion and oedema
- Pulmonary oedema occurs due to venous congestion in the lungs and causes wheezy respirations “Cardiac asthma” Rhonchi, basal crepitations and Chyne-strokes respiration in chronic pulmonary oedema. Cyanosis may be present or not.
- Dyspnoea assessment
- Grade I Breathing feels as good as that of others of own age, sex and build at work, walking, climbing hills or stairs
- Grade II Able to walk with others of own age, sex and build on the levels, unable to keep up on hills or stairs
- Grade III Unable to keep up on level, but able to walk to about one mile or more at own speed.
- Grade IV Unable to more than 100 yards on level without resting due to breathlessness
- Grade V Breathlessness on taking or undressing or inability to leave house because of breathlessness.
- Kidneys
- Reduced cardiac output causes low glomerular filtration rate (GFR) reducing the renal blood flow, which results in renal anoxia and vasoconstriction reflexes. There is sodium retention leading to oedema formation.
- Brain
- Reduced cardiac output compromises blood flow to the brain resulting in cerebral anoxia, irritability, and loss of attention span, restlessness, stupor and coma.
- Liver
- Increased systemic venous pressure causes hepatic congestion (Tender hepatomegaly) with minor abnormalities such increased SGOT, SGPT, serum Bilirubin and abnormalities in BSP excretion
- Autopsy
- Left ventricle is hypertrophied and dilated
- Left atria is dilated
- Mitral ring is enlarged
- Lungs show features of congestion and fluid oedema
Course dashboardClick here to access Unit one Content..
Topic 4.4: RIGHT VENTRICULAR FAILURE (RVF)
- Introduction
- RVF usually combined with LVF and pure RVF occurs in few instances. RVF is usually caused by left ventricular failure (LVF). When caused by pulmonary diseases it is described as the heart of pulmonary disease (cor pulmonale).
- Causes
- Myocardial Infarction (not severe than the left ventricle)
- Chronic Destructive Pulmonary Disease - chronic Bronchitis, emphysema, pulmonary fibrosis, pulmonary abscess and pulmonary tuberculosis (PTB).
- Massive pulmonary embolism
- Pulmonary hypertension following LVF secondary to IHD
- Viral myocarditis
- Constrictive pericarditis
- Valvular lesions (Tricuspid stenosis and congenital pulmonary stenosis)
- Left sided failure
- Congenital heart disease
- Pathology
- Left ventricular failure causes increase left atrial pressure and the pressure in the pulmonary arterial pressure which increases the workload on the right ventricle leading to right ventricular hypertrophy and eventually failure.
- The failing right ventricle is unable to expel all the blood received hence becomes dilated.
- The dilatation results in the stretching of the Tricuspid valve ring leading to Tricuspid regurgitation (incompetence) and blood accumulates in the right atrium, systemic and portal venous systems leading to systemic venous congestion and causing “Cardiac” type of oedema.
- There is increased diastolic volume which causes visceral congestion and effusions, peripheral congestion and oedema (stasis, pitting oedema and distended neck veins).
- Manifestations (Features)
- Primary physiologic disturbance involves damming of blood in the spleenic, systems and portal system and inadequate flow from lungs to left ventricle. Venous congestion and Stagnation occurs throughout the body causing renal anoxia, which results in Sodium and water retention hence increasing the blood volume.
- The Heart - As LVF
- Liver
- Congested and enlarged (hepatomegally). In severe cases there is central haemorrhagic necrosis of liver and healing occurs by formation of a Fibrous tissue a situation that causes “Cardiac Cirrhosis”
- Raised JVP and Oedema
- There is congestion of the peripheral venous system resulting in raised jugular venous pressure and pitting pedal oedema.
- Kidneys
- Congestion and Renal anoxia causes disturbed renal function
- Pedal oedema
- Brain - As in LVF
- Portal system
- Spleen – may become congested and enlarged
- Therefore is a systemic venous congestion syndrome
Course dashboardClick here to access Unit one Content..
Topic 4.5: CONGESTIVE (TOTAL) HEART FAILURE (CCF)
- Introduction
- It involves failure of both Right and Left Ventricles which may fail spontaneously for example in severe myocardial infarction, severe toxic myocarditis e.g. Diphtheria, Beri beri and congestive cardiomyopathy
- Causes
- Increased workload for both ventricles e.g. RHD with lesions involving mitral and Aortic valves
- Increased Cardiac Output e.g. in severe anaemia and thyrotoxicosis (In high output failure - the fall in cardiac output is relative from a previously high cardiac output). But may still be low output failure with an abnormally low output
- Ventricular stiffness that follows poor response to SAN and hypertrophic cardiomyopathy
- NB: Thromboembolic phenomenon is common in CCF due to blood stagnation. This increases the risk of pulmonary embolism
- Low Output Failure – Causes
- Myocardial disease
- Ischaemic heart disease (IHD)
- Myocarditis
- Cardiomyopathy
- Arrthymias
- Hypertension
- Valve stenosis
- Cor pulmonalae
- The cardinal signs of CCF include: -
- Pedal oedema
- Raised JVP
- Tender Hepatomegally
- Cardiomegally
- Gallop rhythm
- Basal crepitations
Course dashboardClick here to access Unit one Content..
Topic 4.6: CCF
- LUNG-HEART INTERACTIONS
- The normal pulmonary circulation is high capacitance, low resistance and the right ventricle is thin. LVF causes pulmonary congestion which decreases PO2 resulting in impaired left ventricular function. Chronic LVF causes chronic pulmonary congestion and vascular changes (pulmonary hypertension) which results in right ventricular hypertrophy (also occur in VSD).
- Right ventricular hypertrophy or pulmonary disease lead to high pulmonary vascular resistance (PVR) resulting in high pulmonary artery and high right ventricular pressures, which affect left ventricular function. Congenital heart disease e.g. VSD causes a left-right shunt which leads to increased right ventricular pressure.
- INVESTIGATIONS OF VENTRICULAR DISEASE
- Chest X-ray (CXR)
- Cardio-thoracic ratio (increased – normal is 0.5)
- Selective enlargement of the atria e.g. in mitral valve disease and severe left ventricular hypertrophy
- Abnormal pulmonary vasculature
- Kerley B Lines
- Pleural effusion (presence of congestion)
- The right border has 3 contours shows the innominate vein and its continuation into the superior vena cava, superior vena cava and the ascending aorta and right atrium. The left border has 3 contours shows aortic arch (knuckles/knob), pulmonary trunk and the main trunk.
- E.C.G shows evidence of ventricular hypertrophy, conduction disturbances, coronary artery disease, left atrial hypertrophy and cardiac arrhythmias
- Echocardiography
- E.C.G phonocardiography - heart sounds & murmurs
- Cardiac catheterisation
- Imaging - CT Scan, MRI
- Mechanocardiography e.g. JVP
- Full haemogram and ESR
- Urea and electrolytes
- Liver biochemistry
Course dashboardClick here to access Unit one Content..
Topic 4: Further Reading
Kishasha M (2016). Textbook of human pathology. 1st edition, Acrodile publishers, Nairobi, Kenya.
Harsh M (2014). Textbook of Pathology. 1st edition. New Delhi: Jaypee Brothers, Medical Pub, India
Ngton C, & Muir (2014). Textbook of Pathology. 15th edition, New Delhi. Jaypee Brothers, India
Course dashboardClick here to access Unit one Content..
Topic 5.1: Ischaemic Heart Disease (IHD)
- Learning Outcomes
- At the end of the lesson the learner should be able to: -
- Define ischaemic heart disease
- Describe blood supply to the heart
- Evaluate risk factors in IHD
- Discuss causes of IHD
- Describe the pathophysiology of IHD
- Explain the effects of IHD
- Discuss the clinical features of IHD
- State the outcome of IHD
- Investigate IHD
- Discuss the complications of IHD
Course dashboardClick here to access Unit one Content..
Topic 5.2: IHD
- INTRODUCTION
- Ischaemic heart disease is a situation when there is diminished myocardial blood supply due to arterial blood flow obstruction or vasoconstriction. It is an acute or chronic state of cardiac disability arising from an imbalance between the supply of oxygen and myocardial demand for these nutrients. Obstruction or narrowing of the coronary arterial system is the most common cause of myocardial anoxia hence the term coronary artery disease is used synonymously with IHD.
- BLOOD SUPPLY TO THE MYOCARDIUM
- Coronary Circulation
- The cardiac muscle functions well when adequately supplied with blood by the coronary arteries originating from the aortic valve during diastole. Any imbalance between this supply and demand causes angina pectoris or/and myocardial infarction.
- The Dominant Artery
- There are two coronary (the left and right coronary artery) arteries responsible for blood supply to the myocardium. The dominant artery is the one that gives off the AV nodal artery and supplies the posterior descending artery. In 95% of males and 85% of females, the right coronary artery is dominant while in the remaining 5% and 15% respectively, the circumflex artery is dominant. Some individuals have collateral channels that connect the major coronary arteries.
- Collateral Circulation
- The coronary arteries are good examples of end arteries but there exits a collateral cardiac and extra-cardiac collateral circulation with a rich anastomososes even though the blood vessels involved are usually very small and can only open if occlusion of the coronary arteries is gradual.
- There is a rich anastomosis of very small vessels between the right and left coronary arteries in the myocardium. The extra-cardiac anastomosis occurs through the pericardium from four pulmonary branches, two caval branches that anastomose with the branches of internal thoracic, bronchial and phrenic arteries.
- Blood Supply Patterns
- There are three anatomic patterns of distribution of coronary blood supply depending on how and which coronary artery crosses the crux (region where all the four heart chambers, interatrial and interventricular septa meet).
- Right dominant system – right coronary artery crosses the crux to supply whole of the right ventricle, posterior half of interventricular septum and part of posterior wall of left ventricle (commonest pattern)
- Balanced cardiac circulation – the right and left coronary arteries supply right and left ventricles respectively, a branch of right coronary artery supplies posterior part of interventricular septum and a branch of the left coronary artery supplies the anterior part.
- Left dominant system - left coronary artery crosses the crux to supply the entire left ventricle, the whole of interventricular septum and part of posterior wall of the right ventricle. (Least frequent pattern).
- Venous Drainage
- Coronary veins run parallel to major coronary arteries draining blood into the coronary sinus, which empties blood directly into the right atrium.
Course dashboardClick here to access Unit one Content..
Topic 5.3: IHD Cont'd
- RISK FACTORS
- Fixed factors e.g. age, male sex and positive family history
- Potentially changeable with treatment
- Strong Association - hyperlipidaemia, cigarette smoking, hypertension and diabetes mellitus
- Weak Association – personality, obesity and physical inactivity, gout, contraceptive pill and heavy alcohol consumption
- AETIOPATHOGENESIS
- .
- IHD is mainly caused by disease affecting coronary arteries which is majorly due to atherosclerosis (90% cases). The aetiology of IHD falls under three broad headings of coronary atherosclerosis, superadded changes in coronary atherosclerosis and non-athersclerotic causes.
CAUSES OF IHD
- Reduced coronary blood flow due to
obstruction
- Atheroma/artherosclerosis (depends on the distribution, location and fixation of the athersclerotic plaques)
- Arterities e.g. inflammation
- Thrombosis – e.g. hypercoagubility states
- Vascular spasms
- Embolus
- Coronary ostial stenosis (e.g. syphilis)
- Coronary arteritis (e.g. polyarteritis)
- Aneurysm – coronary artery
- Trauma - contusion
- Compression - tumours
- Decrease in the flow of oxygenated blood
- Anaemia
- Carbohyhaemaoglobinaemia
- Hypotension – coronary perfusion pressure
- Increased demand for oxygen
- Increased cardiac output - thyrotoxicosis
- Myocardial hypertrophy - aortic Stenosis, hypertension
- PRESENTATION
- The presentation depends on the characteristics of the lesion in the coronary arteries in terms of onset, duration, degree, location and extent. This influences the effects of myocardial ischaemia which may present as: -
- Asymptomatic state
- Angina pectoris
- Myocardial infarctions (acute and chronic)
- Cardiac arrhythmias
- Cardiac Failure
- Sudden death
Course dashboardClick here to access Unit one Content..
Topic 5.4: ANGINA PECTORIS
- INTRODUCTION
- Angina pectoris is a clinical syndrome associated with transient sudden, severe paroxysmal substernal pain due to diminished blood flow through the coronary artery (inadequate perfusion). Angina means strangling. The pain is prompted by exertion, cold and emotional stress and lasts a short time. The pain radiates to the shoulder (jar, check, left arm) and is usually relieved by rest and drugs (vasodilatation -TNT)
- Angina occurs because myocardial cells become ischaemic but the damage is reversible. Reduced blood supply can be as a result of stable or unstable plaques in the vessels. Stable plaques narrow coronary arteries so that blood flow is insufficient for even a moderate increase in cardiac work (e.g. climbing stairs) and the patient complains of chest pain (angina) which is relieved on rest.
- Unstable plaques only produce clinical problems when an acute event occurs causing the fibrous cap of the plaque splits and blood from the lumen can reach the soft necrotic centre. Rupture of the plaque causes distortion and enlargement of the plaque as well as releasing the plaque contents which activate the thrombotic cascade. Platelets and fibrin aggregate blocking the lumen and the platelet constituents (TXA2, histamine and serotonin) promote vasospasm which worsens the situation.
- CAUSES
- Coronary artery disease resulting in impaired perfusion – atheroma, syphilis, valve disorders (AS, AR, severe MS) and vasospasm
- Myocardial infarction - promotes Angina by decreasing blood supply to the surviving myocardium around the infarction. It also relieves angina by eliminating the dead tissue
- PREDISPOSING FACTORS
- The predisposing factors include those that result in increased myocardial oxygen demand such as: -
- Increased ventricular preload e.g. exercise, anaemia and thyrotoxicosis
- Increased ventricular afterload e.g. hypertension, valvular lesions – AS and obstructive cardiomyopathy.
- Increased ventricular wall tension due to dilation and hypertrophy
- Decreased heart function e.g. myocarditis and tachycardia
- Factors Prompting Attacks
- The factors prompting attacks include physical activity, exposure to cold, exercises, injury, shock and coronary artery spasm
- Risks
- The main risk factors are myocardial infarction, cardiac failure and sudden death (ventricular filtration)
- Pathology
- Coronary artery shows arterioscleroses, patchy fibrous intimal thickening, calcification, accumulation of lipid debris and fibrosis
- Myocardium exhibits ischaemic changes and fibrosis
- ECG shows abnormal conduct
- PRESENTATION and CLINICAL PATTERNS OF ANGINA
- There are 3 overlapping clinical patterns of angina pectoris namely stable (typical) angina, Prinzmetal’s variant angina and unstable (crescendo) angina.
- Stable (Typical) Angina
- This is the most common pattern. It is also described as classical or exertional angina. It is characterized by attacks of pain following emotional or physical exertion due to chronic stenosing coronary atherosclerosis and relieved by rest. This is because the coronary artery cannot perfuse the myocardium adequately when the workload on the heart increases. The ECG shows depression of the ST segment due to poor perfusion of the subendocardial region of the left ventricle. There in no elevation of enzymes in blood because there is no irreversible myocardial injury.
- Prinzmetal’s variant Angina
- Variant (Prinzmetal’s) angina is characterized by pain which occurs at rest with no relationship with physical activity. This is mainly due to sudden vasospasm of the coronary trunk induced by coronary atherosclerosis or release of humoral vasoconstrictors by mast cells in the coronary adventitia. The ECG shows ST segment elevation due transmural ischaemia. The patients respond well to vasodilators.
- Unstable (Decrescendo) Angina
- This is also called pre-infarction angina or acute coronary insufficiency due to multiple factors. It is the most serious variety characterized by more frequent onset of pain, prolonged duration pain, often occurring at rest. Indicates impending myocardial infarction and has multiple aetiology.
- INVESTIGATIONS
- ECG
- Coronary angiography
- Chest X-Ray
- VDRL
- Haemogram + ESR
- Echocardiography
Course dashboardClick here to access Unit one Content..
Topic 5.5: MYOCARDIAL INFARCTION cont'd
- Myocardial infarction may present as acute or chromic myocardial infarction. Acute myocardial infarction is the most important consequence of coronary artery disease and many patients die within the first few hours of the onset and the remaining ones suffer impaired cardiac function.
- Diagnosis
- Diagnosis of acute myocardial infarction is based on three types of features – clinical features, ECG changes and serum enzymes determinants.
- Clinical Features
- Chest pain(what characteristics?), indigestion, apprehension, oliguria, low grade fever, shock and acute pulmonary oedema
- ECG Changes
- ST segment elevation
- T wave inversion
- Wide deep Q waves
- Serum cardiac Markers
- Certain proteins and enzymes are released into blood from the necrotic heart muscle after myocardial infarction
- PATHOLOGY
- Structural changes
- Microscopy
- Microscopy
The infarcts have variation in size > 2 cm affecting the inner part of myocardium. Majority of the infarcts are transmural (whole thickness of myocardium). The right coronary artery blockage leads to formation of a posterior, inferior infarct affecting the apex down to the inferior wall of the left ventricle, the adjacent inter-ventricular septum and the adjacent inferior wall of the right ventricle. 15% of the cases involve the left circumflex artery affecting the lateral margins of the left ventricle.
Macroscopy
Congestion (Blotchy congestion)
Pale myocardium
Haemorrhagic margins
Softened patch (dead tissue)
Colour change from grey brown to yellow green
Red zone of vascular granulation (later)
Microscopy
Coagulative necrosis changes
Polymorphonuclearr leucoytes (neutrophils, monocytes)
Digestion of tissues by macrophages
Show necrotic changes at the margins
- DIFFERENTIAL DIAGNOSIS
Aortic dissection
Pulmonary embolism
Spontaneous pneumothorax
Pericarditis
Oesophageal rupture
Peptic Ulcer disease
Pancreatitis
COMPLICATIONS
Arrhythmias due to ventricular fibrillation and heart block especially in the Bundle of His – leads to heart block, ventricular tachycardia and fibrillation or asystole
Cardiac Failure – due to heart block, cell death and valve incompetence
Acute circulatory failure (cardiogenic shock)
Embolism, which can be cerebral or peripheral. Emboli from the left ventricle affect the cerebral, renal, spleenic, femoral artery and deep venous thrombosis (DVT) while those from the right ventricle will affect the pulmonary circulation.
Thrombosis may be atrial, mural or venous
Cardiac aneurysm (ventricular)
Angina pectoris
Recurrence of myocardial infarction
Rupture of infarcted myocardium due to autolytic softening (myomalacia cordia) leading to cardiac tamponade.
Cardiac tamponade
Rupture of inter-ventricular septum
Valve incompetence due to infarction of mitral papillary muscle
Ventricular rapture leading to cardiac tamponade
Post myocardial infarction syndrome (Dressor’s syndrome) which comprise of: - (Persistent fever, Pericarditis and Pleurisy)
Shoulder – Hand syndrome
Pericarditis
- Sudden death
div class="panel-link" data-toggle="modal" data-target="#course-panel">Course dashboardClick here to access Unit one Content..
Topic 5:.6 MYOCARDIAL INFARCTION cont'd
- Myocardial infarction may present as acute or chromic myocardial infarction. Acute myocardial infarction is the most important consequence of coronary artery disease and many patients die within the first few hours of the onset and the remaining ones suffer impaired cardiac function.
- Diagnosis
- Diagnosis of acute myocardial infarction is based on three types of features – clinical features, ECG changes and serum enzymes determinants.
- Clinical Features
- Chest pain(what characteristics?), indigestion, apprehension, oliguria, low grade fever, shock and acute pulmonary oedema
- ECG Changes
- ST segment elevation
- T wave inversion
- Wide deep Q waves
- Serum cardiac Markers
- Certain proteins and enzymes are released into blood from the necrotic heart muscle after myocardial infarction
- PATHOLOGY
- Structural changes
- Microscopy
- Microscopy
The infarcts have variation in size > 2 cm affecting the inner part of myocardium. Majority of the infarcts are transmural (whole thickness of myocardium). The right coronary artery blockage leads to formation of a posterior, inferior infarct affecting the apex down to the inferior wall of the left ventricle, the adjacent inter-ventricular septum and the adjacent inferior wall of the right ventricle. 15% of the cases involve the left circumflex artery affecting the lateral margins of the left ventricle.
Macroscopy
Congestion (Blotchy congestion)
Pale myocardium
Haemorrhagic margins
Softened patch (dead tissue)
Colour change from grey brown to yellow green
Red zone of vascular granulation (later)
Microscopy
Coagulative necrosis changes
Polymorphonuclearr leucoytes (neutrophils, monocytes)
Digestion of tissues by macrophages
Show necrotic changes at the margins
- DIFFERENTIAL DIAGNOSIS
Aortic dissection
Pulmonary embolism
Spontaneous pneumothorax
Pericarditis
Oesophageal rupture
Peptic Ulcer disease
Pancreatitis
COMPLICATIONS
Arrhythmias due to ventricular fibrillation and heart block especially in the Bundle of His – leads to heart block, ventricular tachycardia and fibrillation or asystole
Cardiac Failure – due to heart block, cell death and valve incompetence
Acute circulatory failure (cardiogenic shock)
Embolism, which can be cerebral or peripheral. Emboli from the left ventricle affect the cerebral, renal, spleenic, femoral artery and deep venous thrombosis (DVT) while those from the right ventricle will affect the pulmonary circulation.
Thrombosis may be atrial, mural or venous
Cardiac aneurysm (ventricular)
Angina pectoris
Recurrence of myocardial infarction
Rupture of infarcted myocardium due to autolytic softening (myomalacia cordia) leading to cardiac tamponade.
Cardiac tamponade
Rupture of inter-ventricular septum
Valve incompetence due to infarction of mitral papillary muscle
Ventricular rapture leading to cardiac tamponade
Post myocardial infarction syndrome (Dressor’s syndrome) which comprise of: - (Persistent fever, Pericarditis and Pleurisy)
Shoulder – Hand syndrome
Pericarditis
- Sudden death
Course dashboardClick here to access Unit one Content..
Topic 5.7: Valvular Heart Disease (VHD)
- Learning Outcomes
- At the end of the lesson the learner should be able to: -
- Outline the anatomy of the heart valves
- Describe the causes of valvular damage
- Describe the mechanisms of valvular damage
- Explain the pathology of valve damage
- Explain the clinical presentation of valvular heart disease
- Investigations in valvular heart disease
- Evaluate complications of valvular heart disease
- INTRODUCTION
- Valvular heart diseases comprise of the disorders of the heart valves. Normal function of the heart depends on the mechanical efficiency of the valves whose malfunction contributes immensely to the disability of heart function.
- VALVE DEFORMITY
- A valve deformity can be a stenosis or regurgitation. : Stenosis - a reduction in the valve aperture and increases pressure load in the preceding chambers. Any time there is an obstruction to blood flow across the heart three adjustments may occur: - pressure proximal to the obstruction increases in an attempt to maintain same quality of flow; amount of flow reduces and hence require less pressure difference across the obstruction and duration of flow past the obstruction may be prolonged
- Regurgitation – incompetence of valves that result in failure of the valve to close completely and increases volume load on both sides of the valve
- CAUSES OF DEFORMITY/DISORDERS
- Congenital – usually associated with other congenital disorders
- Acquired - E.g. Rheumatic fever (the commonest cause)
- Post-inflammatory scarring
- Degenerative changes with aging
- Dilatation of the valve ring e.g. in ventricular dilatation
- Degeneration of collagen support tissue of the valve
- Acute destruction by acute necrotizing inflammation
Course dashboardClick here to access Unit one Content..
Topic 5.8: VALVE DEFORMITY
- INTRODUCTION
- Normal function of the mitral valve depends on the mechanical efficiency of the cusp, chordae, papillary muscle, pliability and size of fibrous ring or annules and adequacy of left ventricular contraction. Normal size of circumference is 5 – 12 cm. The valve consists of 2 leaflets (cusps) - a larger anterior leaflet and a small posterior leaflet, annules, the chordae tendineae and papillary muscles

- The mitral valve has a cross-sectional area of 5 cm2 and allows ventricular filling at peak rate of 500 – 1000 mls/s
- Mitral Stenosis (MS)
- Rheumatic Heart disease resulting from acute rheumatic fever is a major cause of mitral stenosis affecting more female than males. In 2/3 cases the aortic valve is also affected
- AETIOLOGY
- Congenital
- Acquired - rheumatic fever /rheumatic heart disease/ (commonest), calcification, infective endocarditis, rheumatoid arthritis and Systemic Lupus Erythromatosus (S.L.E.)
- PATHOPHYSIOLOGY
- Disturbance in left ventricular filling due to reduced mitral valve area (1 - 2.5 cm2), which causes a reduction in peak left ventricular filling rate and loss of normal period of diastasis.
- During exercise as heart rate increases a pressure gradient develops with an increase in mean left atrial pressure in an effort to improve ventricular filling. This will result in left atrial hypertrophy and dilatation.
- There is chronic left atrial hypertension that causes elevation of pulmonary capillary, venous and arterial pressures favouring transudation of fluid resulting in oedema (pulmonary oedema) formation.
- Pulmonary hypertension leads to right ventricular hypertrophy, dilatation and failure.
- There will also be congestion in systemic veins (raised JVP, hepatomegally and pedal oedema).
- There is reduced cardiac output due to poor left ventricular filling and right ventricular failure eventually ending up in cardiac failure.
- PATHOLOGY
- There is distortion of normal mitral valve anatomy with fusion of commisures.
- The cusps:
- Are thickened, distorted and vascularized throughout (normally they are vascularized at the base only)
- Consists of dense fibrous tissue with infiltrations of lymphocytes and plasma cells
- They are fused along the free margins forming a “Button Hole” or “Fish mouth” opening
- There is thrombus formation and calcification
- Great thickening and rigidity causes stenosis and regurgitation
- Chordae - shows thickening, fusion and contraction
- The valve ring is calcified
- CLINICAL FEATURES
- Symptoms
- The symptoms include - reduction in exercise tolerance, breathlessness, fatigue, heaviness of limb, palpitations, cough (productive of blood-tinged, frothy sputum and at times frank haemoptysis), Haemoptysis (due to chest infection, pulmonary infarction, acute pulmonary oedema and rupture of small blood vessels in lungs. Massive or recurrent haemoptysis may be the presenting or only symptom of mitral stenosis.), angina (due to pulmonary hypertension, right ventricular failure and previous coronary embolism), nocturnal dyspnoea (late complain), recurrent chest infection associated with cough, purulent sputum and fluid retention (pulmonary oedema), fluid retention such as pedal oedema, ascites, pleural effusion and pulmonary oedema and features of embolic phenomenon where any organ could be affected.
- Physical Examination (Signs)
- General Examination
- On general examination there is weight loss, peripheral cyanosis, “Malar flash”, the pulse is irregular (Atrial fibrillation), rapid with a normal character (but amplitude may be reduced) or slow rising (small volume, slow rising) and raised JVP if there is right ventricular failure
- The Pericardium
- There is a “tapping apex” due to a palpable first heart sound with a left parasternal heave due to right ventricular hypertrophy. Loud Hs (first heart sound) with a rumbling mid-diastolic murmur/thrill.
- Effects (Other features)
- Left atrial myocardial hypertrophy is limited causing increase in pressure in LA and accumulation of blood in LA and pulmonary veins leading to pulmonary venous congestion. There is also dilatation of the left atrium
- Increased pulmonary venous pressure (PVP) causes pulmonary arterial hypertension leading to right ventricular hypertrophy (RVH) exhibiting features such as dyspnoea, persistent cough, pulmonary oedema, paroxysmal nocturnal dyspnoea (PND) and haemoptysis due to engorged blood vessels
- Right ventricular hypertrophy results in tricuspid regurgitation
- Congestive cardiac failure
- Thrombosis
- Systemic Embolism (worst being cerebral infarction)
- Atrial fibrillation
- Pulmonary hypertension results in pulmonary valve regurgitation that produces an early diastolic murmur (Graham-Steell murmur)
- EFFECTS
- Left atrial dilatation and hypertrophy
- Left ventricular hypertrophy and dilatation
- Diastolic murmur
- INVESTIGATIONS
- Chest X-ray
- Heart size is normal or increased (commonly left atrial enlargement)
- Calcification may be visible
- The Lung fields show dilated veins with an increase in size of main pulmonary artery (pulmonary hypertension)
- Evidence of pulmonary oedema - lymphatic lines, generalized hazy shadowing and obvious interstitial oedema
- Pulmonary haemosiderosis in long standing cases
- E.C.G. shows atrial fibrillation and left atrial hypertrophy (bifid “p” wave)
- Echocardiogram
- Cardiac catheterisation.
- Full haemogram and ESR
- Differential Diagnosis
- 1) Primary pulmonary hypertension
- 2) Left ventricular disease
- COMPLICATIONS
- Atrial fibrillation
- Systemic embolism
- Pulmonary hypertension
- Pulmonary infarction
- Chest infection
- Infective endocarditis
- Tricuspid regurgitation
Course dashboardClick here to access Unit one Content..
Topic 5.9: Mitral Regurgitation (MR)
AETIOLOGY
Rheumatic heart disease (accounts for 50%) and prolapsing mitral valve are the most common causes of mitral regurgitation. Any disorder that causes dilatation of the left ventricle causes mild mitral regurgitation.
Structure Anatomical Pathogenesis
Affected Fault
1. Valve cusps Congenital cleft Atrial Septal Defects (ASD)
Redundant cusps - Marfan’s syndrome,
- Floppy valve syndrome, loss of collagen
Perforation - Infective endocarditis
Distortion/Scarring - Rheumatic fever
Iatrogenic - Floppy Valve
2. Chordae Redundant chordae - Marfan’s syndrome, Floppy valve
Ruptured chordae - Floppy valve, Marfan’s syndrome
- Infective endocarditis/Rheumatic
Chordal shortening - Rheumatic, endomyocardial, fibrosis
3. Papillary muscle Dysfunction - IHD and cardiomyopathy
Prolapsing mitral valve ring - Various
Rupture - Acute myocardial infarction
4. Valve ring Dilatation - severe LV disease
Calcification - Various
- PATHOPHYSIOLOGY
- In pure mitral stenosis, there is a large increase in left ventricular output since the pressure in the left atrium is lower than that in the aorta and resistance to left ventricular ejection is reduced so the stroke volume increases up to three fold. Ejection of blood begins almost immediately after start of ventricular contraction and by the time the aorta valve opens ¼ of the stroke volume has already entered the left atria.
- Incompetence of the mitral valve allows regurgitation of blood into the left atrium during systole producing left atrial dilatation.
- During diastole the additional blood volume freely moves into the left ventricle stretching the left ventricle. This increased volume load leads to left ventricular dilatation and hypertrophy and eventually left ventricular failure.
- Pressure rise in the left atrium during ventricular systole leads to pulmonary congestion and oedema.
- There is increased volume in the atria and ventricle leading to dilatation and hypertrophy of left ventricle.
- CLINICAL FEATURES
- Symptoms - As in mitral stenosis
- Signs
- On palpation of the praecordium, there is a laterally displaced apex beat (diffuse and thrusting). Soft 1st heart sound due to incomplete closure of the heart valves with systolic thrill. A prominent 3rd heart sound resulting from sudden rush of blood into the dilated left ventricle in early systole. Apical pansystolic murmur (regurgitation occurs throughout systole) radiating to axilla
- Effects
- Regurgitation of blood into left atrium during ventricular systole
- Left ventricular Dilatation and Hypertrophy
- Right ventricular hypertrophy and dilatation
- Congestion of the lungs and pulmonary hypertension
- Atrial fibrillation
- Left ventricular failure leading/right ventricular failure/CCF.
- Compensated MR
- The volume in left atria increases during ventricular systole but emptied during diastole with the pressure in the left ventricle remaining about normal (Starling’s Law). In combined MR/MS there is pulmonary congestion, oedema, hypertension (pulmonary) and right ventricular hypertrophy.
- INVESTIGATIONS
- Chest X-ray – shows left atrial and left ventricular enlargement, increased cardio-thoracic ratio (CTR), valve calcification
- ECG (bifid p wave)
- Echocardiogram – dilated left atrium and left ventricle
- Cardiac catheterisation – prominent left atrial systolic pressure
- Full Haemogram + ESR.
Course dashboardClick here to access Unit one Content..
Topic 5.10: THE AORTIC VALVE
- ANATOMY
- The aortic valve consists of 3 semi lunar segments/cusps. The orifice of the aorta surrounds the cusps. There are 2 posterior cusps (the left and right cusp) and one anterior cusp. The cusps are larger, thicker and stronger attachments and opposite the cusps of the aorta there are 3 slight dilatations (Aortic sinuses). Aortic valve disease is a common cause of sudden cardiac deaths.
- Aortic Stenosis (AS)
- INTRODUCTION
- Aortic stenosis is an important cause of cardiac disability that represents a fixed obstruction to the left ventricular ejection at the level of the valve cusps. Aortic stenosis becomes symptomatic when the valve orifice is reduced to 1 cm2 (normal is 3 cm2).
- CAUSES
- Valvular
- Calcified bicuspid valve
- Rheumatic(post inflammatory scarring)
- Senile degeneration (wears & tear) which results from arteriosclerotic degeneration and calcification
- Congenital – Valve with a single commissure and Bicuspid valve
- Infective endocarditis (rare)
- Hyperlipidimea (rare)
- Fixed sub-aortic stenosis (sub-valvular) for example congenital fibrous ridge or diaphragm.
- Supravalvular stenosis e.g. congenital fibrous diaphragm above the aortic valve
- Hypertrophic cardiomyopathy e.g. septal muscle hypertrophy obstructs left ventricular outflow.
- PATHOPHYSIOLOGY
- Pressure resulting from the aortic stenosis leads to development of a pressure gradient between the left ventricular cavity and aorta.
- This resistance is fixed hence differs from the increased peripheral resistance of systemic hypertension which fails during exercise (pressure overload)
- The resultant obstructed left ventricular emptying leads to increased left ventricular pressure and compensatory left ventricular hypertrophy.
- Left ventricular hypertrophy (LVH) causes an increase in the diastolic stiffness of the cavity and therefore end-diastolic pressure increase causing pulmonary vascular congestion.
- The increased ventricular wall thickness (hypertrophy) results in relative ischaemia of left ventricular myocardium leading to – angina, arrthymias and left ventricular failure.
- PATHOLOGY
- Post-Rheumatic aortic stenosis the cusps are thickened, rigid and partly adherent.
- Calcification: - the cusps are thickened by fibrosis, have irregular nodules and are not fussed or vascularized.
- CLINICAL FEATURES
- Symptoms
- There is breathlessness (paroxysmal nocturnal dyspnoea – PND), chest pain due to Ischaemic heart disease (IHD) and angina and syncope
- Signs
- The pulse - Is slow rhythm, low volume, slow rising/plateau; on palpation of the praecordium the apex beat is not usually displaced because hypertrophy (as opposed to dilatation) does not produce noticeable cardiomegally, there is sustained and obvious (heaving) apex beat; systolic thrill on palpation. On auscultation the first heart sound is normal or reduced and a 4th heart sound is present with a systolic murmur that is a low-pitched ejection murmur that radiates to the carotids (Diamond shaped – crescendo-decrescendo pattern).
- Effects
- Left ventricular hypertrophy and dilatation as a result of pressure overload and ischaemia.
- Angina and myocardial infarction
- Ventricular fibrillation
- Pulmonary congestion and oedema
- Right ventricular failure
- Congestive cardiac failure.
- INVESTIGATIONS
- Chest X-ray shows: -
- Left ventricular hypertrophy (LVH) and dilatation
- Dilated aortic root and ascending aorta
- Calcification of the aorta (may be present)
- CTR increases if heart failure is present
- ECG shows: -
- Left ventricular hypertrophy (LVH)
- Bifid “p” wave
- Conduction disturbances such as complete heart block and prolonged PR interval.
- Echocardiogram reveals disruption of normal anatomy of the heart and thickened, calcified and immobile aortic valve
- Cardiac catheterisation.
- Differential Diagnosis
- Hypertrophic cardiomyopathy
- Congenital stenosis
- Heart block
- Fixed sub-valvular stenosis
- Causes of Death
- Pulmonary oedema
- Ventricular fibrillation
- Left ventricular failure (LVF)
Course dashboardClick here to access Unit one Content..
Topic 5.11: Aortic Regurgitation (AR)
- Aortic regurgitation increases the workload
(volume) on the left ventricle.
- The commonest causes are Rheumatic fever and Infective endocarditis.
- CAUSES
- The Cusps
- Distortion of cusps as in rheumatic fever and rheumatoid arthritis
- Perforation of cusps as in infective endocarditis and trauma
- Valve Ring Dilatation - dissecting aneurysm, Marfan’s syndrome, syphilis, Ankylosing spondylitis and Reiter’s syndrome
- Loss of support associated with Ventricular septal defect (VSD)
- Stretching/Distortion of roof of aorta in rheumatic heart disease (RHD), which causes Fibrous thickening and distortion and calcification.
- PATHOPHYSIOLOGY
- There is reflux of blood from the aorta into the left ventricle during diastole
- The total volume of blood pumped into the aorta must increase hence there is increased volume of blood in left ventricle causes increased ventricular mass and size of chamber.
- There is associated with increased left ventricular stroke volume.
- The aortic run off of blood during diastole reduces the diastolic blood pressure compromising coronary perfusion.
- The large ventricular size makes it mechanically less efficient (ischaemic)
- The walls become stiffer and end diastolic pressure increase leading to pulmonary congestion (pulmonary oedema).
- The large stroke volume and peripheral dilatation up-stroke with a larger blood volume leads to a high systolic and low diastolic pressure leading to a bounding pulse or collapsing pulse.
- PATHOLOGY
- In Chronic Rheumatic the Cusps are thickened with fused commisures and have rolled edges with calcification. Thrombosis may be present or absent. In Infective endocarditis the cusps are destroyed and perforation may be present. Spread to the AVN, sinus of vasalva and inter-ventricular septum
- CLINICAL FEATURES
- Symptoms - there is dyspnoea, breathlessness and chest pain (angina pectoris)
- Signs
- The Physical signs due to hyper-dynamic circulation and reflux of blood into left ventricle are pulse is bounding/collapsing/water hammer; Quincke’s sign (capillary pulsation in nail beds), De Musset’s sign (head nodding with each heart beat), Durozier’s sign (systolic bruit over femoral arteries), pistol shot femorals (a sharp bang heard on auscultation over the femoral ) and Corrigan’s sign (visible arterial pulsation in the neck).The apex beat displaced laterally and downwards and there is a diastolic thrill. On auscultation - a high pitched diastolic murmur (Austin Flit murmur)
- Differential Diagnosis
- PDA
- Coronary A – V fistula
- Ruptured sinus of valsalva aneurysm.
- INVESTIGATIONS
- Chest X-ray
- ECG
- Echocardiogram
- Cardiac catheterisation.
- Full haemogram
Course dashboardClick here to access Unit one Content..
Topic 5: Further Reading
Reference Material
- Kishasha M (2016). Textbook of human pathology. 1st edition, Acrodile publishers, Nairobi, Kenya.
- Harsh M (2014). Textbook of Pathology. 1st edition. New Delhi: Jaypee Brothers, Medical Pub, India
- Ngton C, & Muir (2014). Textbook of Pathology. 15th edition, New Delhi. Jaypee Brothers, India
New Programs
- International Studies
- Models & Language Reaching
- Public School Facts
- State Testing Data
- Education Jobs
Latest News
27OCTOBER, 2021
We start our academic term, with a very determine pace...25December, 2021
We release our results...order by votes Up vote 18 Down vote Instead of using a plugin with unnecessary Kbytes, all you need is a simple function like this (see explanation in comments):


