Click here to access Unit one Content..
In order to function, cells require food. On the other hand cell metabolism produces waste products that must be eliminated into the extracellular environment.
Because the plasma membrane separates the intracellular fluid (ICF) from the extracellular fluid (ECF),
All substances that either enter or leave the cell must pass through the plasma membrane• The membrane also keeps valuable proteins and other substances from leaving the cell and prevents the admission of undesirable substances. For this reason; the cell membrane is classified as a semipermeable membrane. (i.e it is permeable or passable to some molecules but impassable to others).
• In general the mechanisms of cellular exchange can be divided into two categories, Active and Passive
• Active require the cell to expend energy (ATP) to effect solute movement across the plasma membrane, whereas passive mechanisms do not require energy expenditure by the cell.
Passive transport
Osmosis
The diffusion of water through a semi-permeable membrane, with the water molecules going from the less concentrated solution to the more concentrated solution.
The dissolved molecules in the more concentrated solution ‘pull’ the water molecules from the less concentrated solution across the semipermeable membrane.
Hypertonic fluids
Contain higher concentration of osmotically active particles than blood plasma.
Hypotonic solutions
Contain a low concentration of osmotically active particles than plasma.
Osmosis is important in maintaining plasma volume, interstitial and intracellular fluid volumes and the other fluid compartments.
When the body retains salt, large amounts of water are also retained.
Isotonic fluids
Contain – Osmotically active particles in the same concentration as found in the plasma of blood. e.g. 0.9% Sodium Chloride in water.
Diffusion
• The constant movement of molecules from a region of relatively higher concentration to one of lower concentration.
• If the substance is equally distributed between two regions, no concentration gradient exists and diffusion equilibrium is present.
• Movement is controlled by interruptions in the membrane called channels or pores. Pores are fluid-filled channels formed by proteins within the membrane.
An example of Diffusion
The movement of oxygen molecules into cells and carbon dioxide molecules out of cells oxygen molecules are being continually consumed by metabolic processes occurring within the cell, so that the concentration gradient favors diffusion of this gas into the cell.
• Carbon dioxide molecules are being continually produced during cellular metabolism, so that the concentration gradient favors diffusion of this gas out of the cell.
Facilitated diffusion
• This is aided by carrier proteins -e.g. integral proteins/ globular proteins act as carriers that transport materials in the opposite direction against their natural direction.
• These carrier proteins are distinguished by two characteristics:-
• Selectivity
• Gates
Selectivity
• Due to characteristic of channel such as diameter, shape and nature of electrical charges on the inner surface.
Example sodium channels are 0.3 by o.5 nanometer and the fact that the inner surface is negatively charged.
• Potassium channels are 0.3 by 0.3
Gates
• Channels are opened and closed by gates.
• The opening and closing of gates are controlled by two principal ways;
Voltage gating :
This is where the gate responds to the electric potential across the cell membrane.
Ligand gating :
Caused by the binding of another molecule with the protein, this causes conformational change in the protein leading to opening or closing of the gates is referred to as ligand gating.
E.g. acetylcholine an excitatory neurotransmitter. it allows movement of positively charged sodium ions and transmission of impulse.(enables impulse to leap junction)
Factors that may affect diffusion
Permeability of membrane due to;
• Thickness of membrane
• Lipid solubility
• Number of protein channels
• Temperature- increased temperature. Causes increased rate of diffusion.
• Molecular weight of a substance
Concentration difference of diffusing substance.
Effect of electrical potential on diffusion of ions i.e. between the two sides of the membrane
The pressure difference across the membrane movement of substance occur from high to low pressure
Filtration
• Filtration, the passage of water containing dissolved materials through a membrane as a result of a mechanical force on one side.
• E.g. of filtration in the human body is the formation of urine in the microscopic functional units of the kidney.
Active Transport
Often molecules move into or out of living cell in an opposite direction from the way in• which they would normally flow by diffusion
• I.e. move from an area where they are in relatively lower concentration.
• This movement because it is against the natural flow, requires energy in the form of ATP. It also requires proteins in the cell membrane that act as carriers for the molecules.
• This process allows the cell to take in what it needs from the surrounding fluids and to release materials from the cell.
• Cell membrane is described as selectively permeable based on the needs of the cell.
Endocytosis and Exocytosis
• These are methods of bringing particles into the cell and releasing secretions to the exterior of the cell.
Endocytosis refers to the bringing in of protein and other substances through invagination of the outer cell membrane. The process occurs in the following ways:
Pinocytosis (Solution) / “Cell drinking”
• Involves movement of complex proteins and some strong electrolyte solutions into the cell.
• The protein is seen to adhere to the outer cell membrane, which stimulates invagination of the membrane.
• The material is enclosed in a vesicle and floats into the cytoplasm.
• Lysosomes attach to the vesicle, surface, release hydrolytic enzymes into the vesicle, and the enzymes break down the complex material for use within the cells. Substances ingested are in solution hence not visible under the microscope.
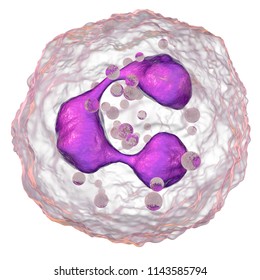
Phagocytosis ‘cell eating’
• The process by which bacteria, dead tissue or other bits of material visible under the microscope are engulfed by cells such as the polymorhonuclear leucocytes of the blood.
The material makes contact with the cell membrane, which then invaginates. The invagination is pinched off, leaving the engulfed material in the membrane – enclosed vacuole and the cell membrane intact.Exocytosis (“Emeocytosis – (“Cell vomiting”)
• This has been called reverse pinocytosis and is an active release of soluble products to the ECF.
• Proteins that are secreted by cells move from the endoplasmic reticulum to the Golgi complex. Where they are packaged into secretory granules..
• To be secreted the granules adhere to the inner cell membrane. The area of fusion breaks leaving the contents of the granule outside the cell and the cell membrane intact. EXAMPLE-secretion of waste products from cell, or release of neurotransmitters.
• NB Both endocytosis and exocytosis require energy and are affected by cellular ability to synthesize ATP.
The Sodium-Potassium pump
Referred to as Sodium-Potassium –activated adenosine triphosphatase (Naa-K+ Atpase).
It’s an active transport mechanism which pumps sodium outward through the cell membrane and at the same time pumps potassium from the outside to the inside.
• The Sodium-Potassium pump responsible for the coupled active transport of Na+ out of cells and K+ into cells is a unique protein in the cell membrane.
• This protein is also an adenosine triphosphatase i.e. an enzyme that catalyze the hydrolysis of ATP to Adenosine diphosphate (ADP) its activated by Na+ and K+.
• The pump extrudes 3Na+ from cells for each two K+ it takes into the cell. Ration3/2.The carrier protein (molecular weight 100,000)
The carrier protein (molecular weight 100,000), Has 3 receptor sites for binding to Na+ on a part that protrudes to the interior cell. Has 2 receptor sites for K+ binding on the outside.• The inside portion of this protein (near the Na+ binding site) has an Atpase activity.
• The amount of Na+ extruded by cell is partly regulated in a feedback by the amount of Na+ in the cell. When 3Na+ bind on the inside of the carrier protein and 2K+ on the outside the Atpase becomes activated
• This cleaves one molecule of ATP to split to ADP –liberating energy which aid in in extruding Na+ to the outside and potassium to the inside.
Functions of the sodium-potassium pump
• It’s present in all cells of the body.
• Responsible for establishing a negative electrical potential inside the cells.
• It is the basis of Nerve function to transmit nerve signals across the nervous system.
• The Sodium-potassium pump contributes to the membrane potential.
• controls cell volume, regulates water volume (osmosis of water to interior cell may lead to cell burst this is prevented by the movement 3 sodium that moves together with water to the exterior of the cell.
Resting membrane potential in transport
Resting membrane potential (Steady potential.)
There is a potential difference across the membranes of most of cells, with the inside of the cells Negative to the exterior there are channels via which ions pass
• The channels for Na+ K+ and Cl are all different.
• The Sodium-potassium pump contributes to the membrane potential.
• It maintains the concentration gradient on which the membrane potential depends.
• If the resting membrane potential is decreased by the passage of a current through the membrane, the electrical gradient that keeps K+ inside the cell is decreased, and there is an increase in K+ diffusion out of the cell.